Immunomodulatory Activity of a Colony-stimulating Factor-1 Receptor Inhibitor in Patients with Advanced Refractory Breast or Prostate Cancer: A Phase I Study.

Purpose: Tumor-associated macrophages correlate with increased invasiveness, growth, and immunosuppression. Activation of the colony-stimulating factor-1 receptor (CSF-1R) results in proliferation, differentiation, and migration of monocytes/macrophages. This phase I study evaluated the immunologic and clinical activity, and safety profile of CSF-1R inhibition with the mAb LY3022855.
Patients and methods: Patients with advanced refractory metastatic breast cancer (MBC) or metastatic castration-resistant prostate cancer (mCRPC) were treated with LY3022855 intravenously in 6-week cycles in cohorts: (A) 1.25 mg/kg every 2 weeks (Q2W); (B) 1.0 mg/kg on weeks 1, 2, 4, and 5; (C) 100 mg once weekly; (D)100 mg Q2W. mCRPC patients were enrolled in cohorts A and B; patients with MBC were enrolled in all cohorts. Efficacy was assessed by RECIST and Prostate Cancer Clinical Trials Working Group 2 criteria.
Results: Thirty-four patients (22 MBC; 12 mCRPC) received ≥1 dose of LY3022855. At day 8, circulating CSF-1 levels increased and proinflammatory monocytes CD14DIMCD16BRIGHT decreased. Best RECIST response was stable disease in five patients with MBC (23%; duration, 82-302 days) and three patients with mCRPC (25%; duration, 50-124 days). Two patients with MBC (cohort A) had durable stable disease >9 months and a third patient with MBC had palpable reduction in a nontarget neck mass. Immune-related gene activation in tumor biopsies posttreatment was observed. Common any grade treatment-related adverse events were fatigue, decreased appetite, nausea, asymptomatic increased lipase, and creatine phosphokinase.
Conclusions: LY3022855 was well tolerated and showed evidence of immune modulation. Clinically meaningful stable disease >9 months was observed in two patients with MBC.
Prospective Multicenter Study of Circulating Tumor Cell AR-V7 and Taxane Versus Hormonal Treatment Outcomes in Metastatic Castration-Resistant Prostate Cancer
Purpose: Androgen receptor splice variant 7 (AR-V7) detection in circulating tumor cells (CTCs) is associated with a low probability of response and short progression-free (PFS) and overall survival (OS) in men with metastatic castration-resistant prostate cancer (mCRPC) treated with enzalutamide or abiraterone. However, it is unclear whether such men benefit from taxane chemotherapy.
Patients and methods: PROPHECY is a multicenter prospective blinded study of patients with poor-risk mCRPC starting abiraterone or enzalutamide and observed through subsequent progression and taxane chemotherapy. We assessed AR-V7 status using the Johns Hopkins modified AdnaTest CTC AR-V7 messenger RNA assay and the Epic Sciences CTC nuclear-localized AR-V7 protein assay before treatment. The primary objective was to validate the independent prognostic value of CTC AR-V7 status based on radiographic/clinical PFS. OS, confirmed prostate-specific antigen (PSA), and objective radiologic responses were secondary end points.
Results: We enrolled 118 men with mCRPC treated with abiraterone or enzalutamide, 51 of whom received subsequent docetaxel or cabazitaxel. Pretreatment CTC AR-V7 status by the Johns Hopkins and Epic Sciences assays was independently associated with worse PFS (hazard ratio [HR], 1.7; 95% CI, 1.0 to 2.9 and HR, 2.1; 95% CI, 1.0 to 4.4, respectively) and OS (HR, 3.3; 95% CI, 1.7 to 6.3 and HR, 3.0; 95% CI, 1.4 to 6.3, respectively) and a low probability of confirmed PSA responses, ranging from 0% to 11%, during treatment with abiraterone or enzalutamide. At progression, subsequent CTC AR-V7 detection was not associated with an inferior PSA or radiographic response or worse PFS or OS with subsequent taxane chemotherapy after adjusting for CellSearch CTC enumeration and clinical prognostic factors.
Conclusion: Detection of AR-V7 in CTCs by two different blood-based assays is independently associated with shorter PFS and OS with abiraterone or enzalutamide, but such men with AR-V7-positive disease still experience clinical benefits from taxane chemotherapy.
Circulating tumour cell enumeration does not correlate with Miller-Payne grade in a cohort of breast cancer patients undergoing neoadjuvant chemotherapy

Purpose: The association between pathological complete response (pCR) in patients receiving neoadjuvant chemotherapy (NAC) for breast cancer and Circulating Tumour Cells (CTCs) is not clear. The aim of this study was to assess whether CTC enumeration could be used to predict pathological response to NAC in breast cancer as measured by the Miller-Payne grading system.
Methods: Twenty-six patients were recruited, and blood samples were taken pre- and post-NAC. CTCs were isolated using the ScreenCell device and stained using a modified Giemsa stain. CTCs were enumerated by 2 pathologists and classified as single CTCs, doublets, clusters/microemboli and correlated with the pathological response as measured by the Miller-Payne grading system. χ2 or ANOVA was performed in SPSS 24.0 statistics software for associations.
Results: 89% of patients had invasive ductal carcinoma (IDC) and 11% invasive lobular carcinoma (ILC). At baseline 85% of patients had CTCs present, median 7 (0-161) CTCs per 3 ml of whole blood. Post-chemotherapy, 58% had an increase in CTCs. This did not correlate with the Miller-Payne grade of response. No significant association was identified between the number of CTCs and clinical characteristics; however, we did observe a correlation between pre-treatment CTC counts and body mass index, p < 0.05. Conclusions: Patients with a complete response to NAC still had CTCs present, suggesting enumeration is not sufficient to aid surgery stratification. Additional characterisation and larger studies are needed to further characterise CTCs isolated pre- and post-chemotherapy. Long-term follow-up of these patients will determine the significance of CTCs in NAC breast cancer patients.
Cytopathological Heterogeneity of Circulating Tumor Cells in Non-metastatic Esophageal Adenocarcinoma
Background/aim: The presence of circulating tumor cells (CTC) has been reported to have an impact on prognosis in different tumor entities. Little is known about CTC morphology and heterogeneity.
Patients and methods: In a multicenter setting, pre-therapeutic peripheral blood specimens were drawn from patients with non-metastatic esophageal adenocarcinoma (EAC). CTCs were captured by size-based filtration (ScreenCell®), subsequently Giemsa-stained and evaluated by two trained readers. The isolated cells were categorized in groups based on morphologic criteria.
Results: Small and large single CTCs, as well as CTC-clusters, were observed in 69.2% (n=81) of the 117 specimens; small CTCs were observed most frequently (59%; n=69), followed by large CTCs (40%; n=47) and circulating cancer-associated macrophage-like cells (CAMLs; 34.2%, n=40). Clusters were rather rare (12%; n=14). CTC/CAML were heterogeneous in the cohort, but also within one specimen. Neither the presence of the CTC subtypes/CAMLs nor the exact cell count were associated with the primary clinical TNM stage.
Conclusion: Morphologically heterogenic CTCs and CAMLs are present in patients with non-metastatic, non-pretreated EAC.
Cluster circulating tumor cells in surgical cases of lung cancer
Bladder cancer (BC) is one of the most expensive lifetime cancers to treat because of the high recurrence rate, repeated surgeries, and long-term cystoscopy monitoring and treatment. The lack of an accurate classification system predicting the risk of recurrence or progression leads to the search for new biomarkers and strategies. Our pilot study aimed to identify a prognostic gene signature in circulating tumor cells (CTCs) isolated by ScreenCell devices from muscle invasive and non-muscle invasive BC patients. Through the PubMed database and Cancer Genome Atlas dataset, a panel of 15 genes modulated in BC with respect to normal tissues was selected. Their expression was evaluated in CTCs and thanks to the univariate and multivariate Cox regression analysis, EGFR, TRPM4, TWIST1, and ZEB1 were recognized as prognostic biomarkers. Thereafter, by using the risk score model, we demonstrated that this 4-gene signature significantly grouped patients into high- and low-risk in terms of recurrence free survival (HR = 2.704, 95% CI = 1.010−7.313, Log-rank p < 0.050). Overall, we identified a new prognostic signature that directly impacted the prediction of recurrence, improving the choice of the best treatment for BC patients.
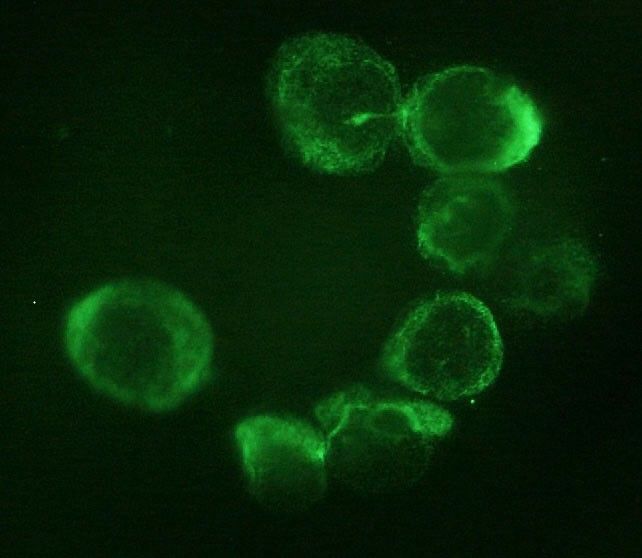
Isolation and Enumeration of CTC in Colorectal Cancer Patients: Introduction of a Novel Cell Imaging Approach and Comparison to Cellular and Molecular Detection Techniques
Despite significant progress in screening and treatment regimens, colorectal cancer
(CRC) still is a major health burden lacking profound liquid biomarkers for identifying patients at risk.
Circulating tumour cells (CTC) have the potential to non-invasively improve the diagnosis. We have
already established a sensitive semi-quantitative RT-qPCR against CK20 for CTC quantification in
CRC patients. For clinical translation, this study aims to validate our molecular detection method by
terms of cytological approaches, and implement a novel semi-automated microscopic detection after
immunofluorescence labelling of CTC. Additionally, we aim to compare our PCR-based approach to
a marker-independent, but size-dependent, enrichment process. We have successfully applied the
validation techniques and proved their feasibility. Enumeration by size yielded the highest numbers
of CTC and demonstrated to be the most reliable strategy for CTC detection in CRC patients. Future
studies with larger patient cohorts will have to investigate the clinical significance and prognostic
value of this approach.
Comparative performance of different methods for circulating tumor cell enrichment in metastatic breast cancer patients

The isolation and analysis of circulating tumor cells (CTC) has the potential to provide minimally invasive diagnostic, prognostic and predictive information. Widespread clinical implementation of CTC analysis has been hampered by a lack of comparative investigation between different analytic methodologies in clinically relevant settings. The objective of this study was to evaluate four different CTC isolation techniques-those that rely on surface antigen expression (EpCAM or CD45 using DynaBeads® or EasySep™ systems) or the biophysical properties (RosetteSep™ or ScreenCell®) of CTCs. These were evaluated using cultured cells in order to calculate isolation efficiency at various levels including; inter-assay and inter-operator variability, protocol complexity and turn-around time. All four techniques were adequate at levels above 100 cells/mL which is commonly used for the evaluation of new isolation techniques. Only the RosetteSep™ and ScreenCell® techniques were found to provide adequate sensitivity at a level of 10 cells/mL. These techniques were then applied to the isolation and analysis of circulating tumor cells blood drawn from metastatic breast cancer patients where CTCs were detected in 54% (15/28) of MBC patients using the RosetteSep™ and 75% (6/8) with ScreenCell®. Overall, the ScreenCell® method had better sensitivity.
Genomic Analysis of Localized High-Risk Prostate Cancer Circulating Tumor Cells at the Single-Cell Level
Accurate risk classification of men with localized high-risk prostate cancer directly affects treatment management decisions and patient outcomes. A wide range of risk assessments and classifications are available. However, each one has significant limitations to distinguish between indolent and aggressive prostate cancers. Circulating tumor cells (CTCs) may provide an alternate additional source, beyond tissue biopsies, to enable individual patient-specific clinical assessment, simply because CTCs can reveal both tumor-derived and germline-specific genetic information more precisely than that gained from a single diagnostic biopsy. In this study, we combined a filtration-based CTC isolation technology with prostate cancer CTC immunophenotyping to identify prostate cancer CTCs. Next, we performed 3-D telomere profiling prior to laser microdissection and single-cell whole-exome sequencing (WES) of 21 CTCs and 4 lymphocytes derived from 10 localized high-risk prostate cancer patient samples. Localized high-risk prostate cancer patient CTCs present a high number of telomere signals with lower signal intensities (short telomeres). To capture the genetic diversity/heterogeneity of high-risk prostate cancer CTCs, we carried out whole-exome sequencing. We identified 202,241 single nucleotide variants (SNVs) and 137,407 insertion-deletions (indels), where less than 10% of these genetic variations were within coding regions. The genetic variation (SNVs + indels) and copy number alteration (CNAs) profiles were highly heterogeneous and intra-patient CTC variation was observed. The pathway enrichment analysis showed the presence of genetic variation in nine telomere maintenance pathways (patients 3, 5, 6, and 7), including an important gene for telomere maintenance called telomeric repeat-binding factor 2 (TRF2). Using the PharmGKB database, we identified nine genetic variations associated with response to docetaxel. A total of 48 SNVs can affect drug response for 24 known cancer drugs. Gene Set Enrichment Analysis (GSEA) (patients 1, 3, 6, and 8) identified the presence of CNAs in 11 different pathways, including the DNA damage repair (DDR) pathway. In conclusion, single-cell approaches (WES and 3-D telomere profiling) showed to be useful in unmasking CTC heterogeneity. DDR pathway mutations have been well-established as a target pathway for cancer therapy. However, the frequent CNA amplifications found in localized high-risk patients may play critical roles in the therapeutic resistance in prostate cancer.
Detection of circulating tumor cells in patients with laryngeal cancer using ScreenCell: Comparative pre- and post-operative analysis and association with prognosis
The presence of circulating tumor cells (CTCs) in the blood of patients with metastatic breast, colorectal and prostate cancer have been widely investigated; however, few studies have examined CTCs in patients with laryngeal cancer. The present pilot study aimed to detect pre- and postoperative CTCs in the blood of patients with laryngeal cancer and evaluate the association with prognosis. Eight patients with laryngeal squamous cell carcinoma (LSCC) at stage III were included in the present study and underwent total or subtotal laryngectomy and radical bilateral neck lymph node dissection. Blood samples were collected from all patients before and after surgery at different time-points. The following processing steps were followed; preoperative blood sampling, surgery, postoperative blood sampling at 3, 6 and 12 month follow-ups, and prognostic association analysis. CTCs were retained on ScreenCell filters for cytological characterization. The presence of CTCs was associated with a less favorable prognosis, whereas a decrease of CTCs in the postoperative sampling was observed in patients who exhibited an improved therapeutic response. The results of the present pilot study revealed a possible association between the presence of CTCs and a less favorable prognosis in patients with LSCC; therefore, these preliminary findings may encourage further research into the incorporation of a liquid biopsy in the management of LSCC, as this may help identify patients with occult metastatic disease earlier and in a non-invasive manner. In addition, this approach may represent novel independent prognostic factor for use in the clinical evaluation of patients with LSCC.
Platinum-Based Chemotherapy in Metastatic Prostate Cancer With DNA Repair Gene Alterations

Purpose: Alterations in DNA damage repair (DDR) genes occur in up to 25% of patients with metastatic castration-resistant prostate cancer (mCRPC) and may sensitize to platinum chemotherapy. We aimed to evaluate the efficacy of platinum-based chemotherapy in DDR-mutant (DDRmut) mCRPC.
Methods: We assessed response to platinum chemotherapy based on DDR gene alteration status in men with mCRPC who underwent tumor and germline genomic profiling. Patients with deleterious alterations in a gene panel that included BRCA2, BRCA1, ATM, PALB2, FANCA, and CDK12 were considered DDRmut.
Results: A total of 109 patients with mCRPC received platinum-based chemotherapy between October 2013 and July 2018. Sixty-four of 109 patients were taxane refractory and poly (ADP-ribose) polymerase inhibitor (PARPi) naïve. Within this subset, DDRmut was found in 16/64 patients (25%) and was associated with an increased likelihood of achieving a prostate-specific antigen (PSA) decline of 50% or more from baseline (PSA50; odds ratio, 7.0; 95% CI, 1.9 to 29.2). Time on platinum chemotherapy tended to be longer in the DDRmut group (median, 3.0 v 1.6 months; hazard ratio, 0.55, 95% CI, 0.29 to 1.24). No difference in survival was detected. Of 8 patients with DDRmut disease who received platinum-based therapy after a PARPi, 3/7 evaluable patients had radiographic partial response or stable disease, and 2/7 had a PSA50 response. None of 4 patients with ATM mutations had platinum responses regardless of prior PARPi exposure.
Conclusion: Patients with DDRmut disease had better response to platinum-based chemotherapy, suggesting that DDR status warrants prospective validation as a potential biomarker for patient selection. Responses to platinum chemotherapy were observed in BRCA-altered prostate cancer after PARPi progression. Additional studies are needed to determine the predictive role of individual genes on platinum sensitivity in the context of other clinical and genomic factors.