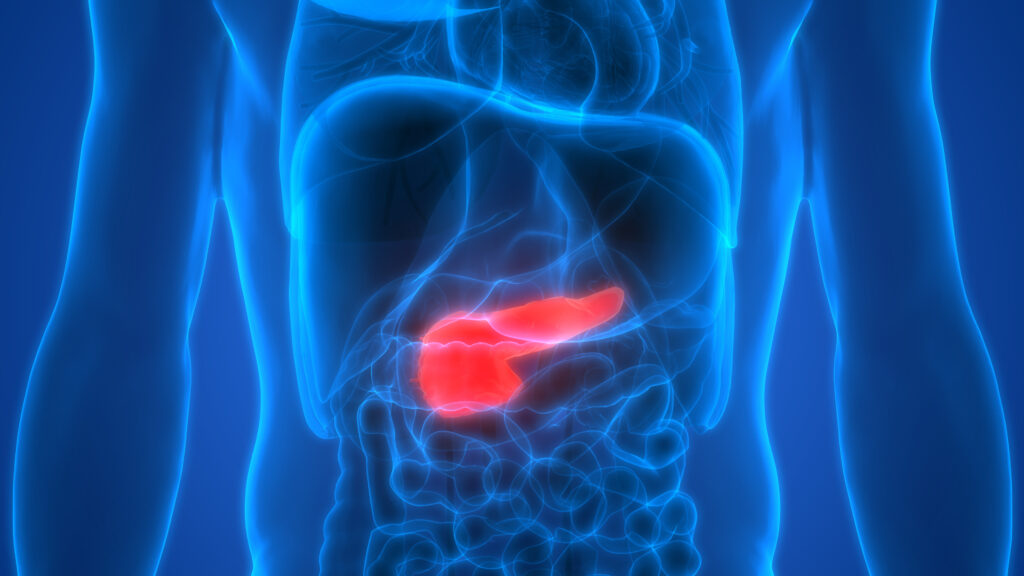
Usefulness of circulating tumor cell detection in pancreatic adenocarcinoma diagnosis
No abstract available
Circulating tumor cells found in patients with localized and advanced pancreatic cancer
Objectives
Isolation of circulating tumor cells (CTCs) holds the promise of diagnosing and molecular profiling cancers from a blood sample. Here, we test a simple new low-cost filtration device for CTC isolation in patients with pancreatic ductal adenocarcinoma (PDAC).
Methods
Peripheral blood samples drawn from healthy donors and PDAC patients were filtered using ScreenCell devices, designed to capture CTCs for cytologic and molecular analysis. Giemsa-stained specimens were evaluated by a pancreatic cytopathologist blinded to the histological diagnosis. Circulating tumor cell DNA was subjected to KRAS mutational analysis.
Results
Spiking experiments demonstrated a CTC capture efficiency as low as 2 cells/mL of blood. Circulating tumor cells were identified by either malignant cytology or presence of KRAS mutation in 73% of 11 patients (P = 0.001). Circulating tumor cells were identified in 3 of 4 patients with early (≤American Joint Committee on Cancer stage IIB) and in 5 of 7 patients with advanced (≥ American Joint Committee on Cancer stage III) PDAC. No CTCs were detected in blood from 9 health donors.
Conclusions
Circulating tumor cells can be found in most patients with PDAC of any stage, whether localized, locally advanced, or metastatic. The ability to capture, cytologically identify, and genetically analyze CTCs suggests a possible tool for the diagnosis and characterization of genetic alterations of PDAC.
Expression Profiling of Circulating Tumor Cells in Pancreatic Ductal Adenocarcinoma Patients: Biomarkers Predicting Overall Survival

The interest in liquid biopsy is growing because it could represent a non-invasive prognostic or predictive tool for clinical outcome in patients with pancreatic ductal adenocarcinoma (PDAC), an aggressive and lethal disease. In this pilot study, circulating tumor cells (CTCs), CD16 positive atypical CTCs, and CTC clusters were captured and characterized in the blood of patients with PDAC before and after palliative first line chemotherapy by ScreenCell device, immunohistochemistry, and confocal microscopy analysis. Gene profiles were performed by digital droplet PCR in isolated CTCs, five primary PDAC tissues, and three different batches of RNA from normal human pancreatic tissue. Welsh’s t-test, Kaplan-Meier survival, and Univariate Cox regression analyses have been performed. Statistical analysis revealed that the presence of high CTC number in blood is a prognostic factor for poor overall survival and progression free survival in advanced PDAC patients, before and after first line chemotherapy. Furthermore, untreated PDAC patients with CTCs, characterized by high ALCAM, POU5F1B, and SMO mRNAs expression, have shorter progression free survival and overall survival compared with patients expressing the same biomarkers at low levels. Finally, high SHH mRNA levels are negatively associated to progression free survival, whereas high vimentin mRNA levels are correlated with the most favorable prognosis. By hierarchical clustering and correlation index analysis, two cluster gene signatures were identified in CTCs: the first, with high expression of VEGFA, NOTCH1, EPCAM, IHH, is the signature of PDAC patients before chemotherapy, whereas the second, with an enrichment in the expression of CD44, ALCAM, and POU5F1B stemness and pluripotency genes, is reported after palliative chemotherapy. Overall our data support the clinic value of the identification of CTC’s specific biomarkers to improve the prognosis and the therapy in advanced PDAC patients.
KRAS mutations in pancreatic circulating tumor cells: a pilot study
Cytologic Characteristics of Circulating Epithelioid Cells in Pancreatic Disease

Background—Circulating epithelioid cells (CECs), also known as circulating tumor/cancer/
epithelial/non-hematologic cells, are a prognostic factor in various malignancies that can be
isolated via various protocols. We analyzed the cytomorphologic characteristics of CECs isolated
by size in a cohort of patients with benign and malignant pancreatic diseases to determine if
cytomorphological features could predict CEC origin.
Methods—Blood samples were collected from 9 healthy controls and 171 patients with
pancreatic disease presenting for surgical evaluation prior to treatment. Blood was processed with
the ScreenCell size-based filtration device. Evaluable CECs were analyzed in a blinded fashion for
cytomorphologic characteristics including cellularity, nucleoli, nuclear size/irregularity/variability/
hyperchromasia, and nuclear-cytoplasmic ratio. Statistical differences between variables were
analyzed via Fisher’s exact test.
Results—No CECs were identified in normal healthy controls (n=9). Of the 115 patients with
CECs (positive or suspicious), 25 had non-malignant disease and 90 had malignancy. There were
no significant differences in any of the cytologic criteria between groups divided by benign versus
malignant, neoplastic versus non-neoplastic, or pancreatic ductal adenocarcinoma versus
neuroendocrine tumor.
Conclusions—CECs were seen in patients with malignant and non-malignant pancreatic
disease, but not in healthy controls. There were no morphologic differences between cells from
different pancreatic diseases. This suggests that numerous conditions may be associated with
CECs in the circulation and that care must be taken not to over-interpret cells identified by
cytomorphology as indicative of circulating tumor cells of pancreatic cancer. Additional studies
are required to determine the origin and clinical significance of these cells.
Circulating Epithelial Cells in Patients with Pancreatic Lesions:Clinical and Pathologic Findings
Background: Circulating epithelial cell (CEC) isolation has provided diagnostic and prognostic information for a variety of cancers, previously supporting their identity as circulating tumor cells in the literature. However, we report CEC findings in patients with benign, premalignant, and malignant pancreatic lesions using a size-selective filtration device.
Study design: Peripheral blood samples were drawn from patients found to have pancreatic lesions on preoperative imaging at a surgical clinic. Blood was filtered using ScreenCell devices, which were evaluated microscopically by a pancreatic cytopathologist. Pathologic data and clinical outcomes of these patients were obtained from medical records during a 1-year follow-up period.
Results: Nine healthy volunteers formed the control group and were found to be negative for CECs. There were 179 patients with pancreatic lesions that formed the study cohort. Circulating epithelial cells were morphologically similar in patients with a variety of pancreatic lesions. Specifically, CECs were identified in 51 of 105 pancreatic ductal adenocarcinomas (49%), 7 of 11 neuroendocrine tumors (64%), 13 of 21 intraductal papillary mucinous neoplasms (62%), and 6 of 13 patients with chronic pancreatitis. Rates of CEC identification were similar in patients with benign, premalignant, and malignant lesions (p = 0.41). In addition, CEC findings in pancreatic ductal adenocarcinoma patients were not associated with poor prognosis.
Conclusions: Although CECs were not identified in healthy volunteers, they were identified in patients with benign, premalignant, and malignant pancreatic lesions. The presence of CECs in patients presenting with pancreatic lesions is neither diagnostic of malignancy nor prognostic for patients with pancreatic ductal adenocarcinoma.